What is shingles?
Shingles, or Herpes zoster, is is caused by reactivation of the Varicella Zoster Virus (the same virus that causes Chicken pox). Shingles typically presents as an itchy, blistering rash. This rash appears either on the right or left side of the body, not crossing the middle. It can develop on your torso or head (including eyes), most commonly appearing on the chest or abdomen.1
People have described shingles pain as burning, stabbing or shock-like. It can disrupt your life, affecting daily activities like getting dressed, walking and sleeping.1,2
Along with the rash and pain, you could also experience sensitivity to light and touch, headache and not feeling well.1
What you need to know about shingles
Don’t underestimate shingles
Shingles pain can be excruciating. It can feel like burning, stabbing or shock-like. The pain can make even simple daily tasks challenging.1,4
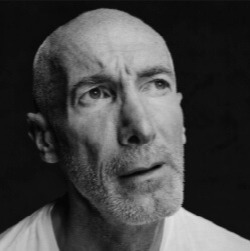

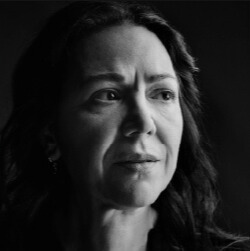

All images across the webpage are patient portrayals.
References
- Harpaz R, Ortega-Sanchez IR, Seward JF. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008;57(RR-5):1–30.
- Weinke T, Edte A, Schmitt S, Lukas K. Impact of herpes zoster and post-herpetic neuralgia on patients’ quality of life: a patient-reported outcomes survey. Z Gesundh Wiss. 2010;18:367–374.
- HSE advice on shingles Shingles: symptoms, causes, diagnosis and treatments - HSE.ie last accessed August 2025.
- Bollaerts K, Riera-Montes M, Heininger U, et al. A systematic review of varicella seroprevalence in European countries before universal childhood immunization: deriving incidence from seroprevalence data. Epidemiol Infect. 2017;145:2666–2677.
- Kawai K et al. BMJ Open. 2014 Jun 10;4(6):e004833. doi: 10.1136/bmjopen-2014-004833
- Lee C, Giannelos N, Curran D, et al. Lifetime risk of herpes zoster in the population of Beijing, China. Public Health Pract (Oxf). 2023;5:100356.
- Södergren E, Mårdberg K, Nishimwe M, et al. Incidence and burden of herpes zoster in Sweden: a regional population-based register study. Infect Dis Ther. 2024;13(1):121–140.
- Hales CM, Harpaz R, Ortega-Sanchez I, Bialek SR. Update on recommendations for use of herpes zoster vaccine. MMWR Morb Mortal Wkly Rep. 2014;63(33):729–731.
If you experience any side effects while taking a medicinal product, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. Adverse events should be reported directly to the Health Products Regulatory Authority (HPRA) on their website: Reporting Suspected Side Effects (hpra.ie)